Uncontrolled diabetes mellitus is a significant risk factor for complications of diabetes, including cardiovascular disease.
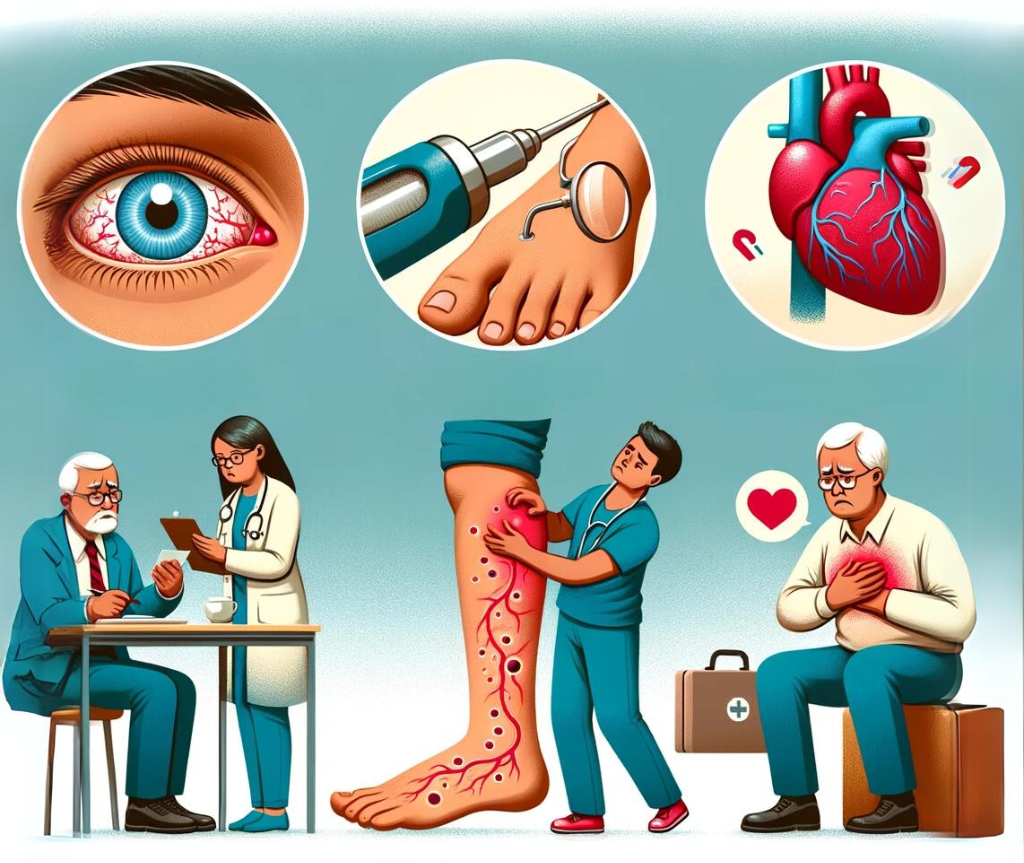
Microvascular disease is when tiny blood vessels in the body get damaged due to high blood glucose levels. This can harm different organs, like the eyes (diabetic retinopathy), nerves (diabetic neuropathy), and kidneys (diabetic nephropathy).
Diabetes can also damage bigger blood vessels, which is called macrovascular disease. This can affect the blood vessels in the heart and brain and make it more likely to have a heart attack, stroke, or a disease in the legs called peripheral arterial disease.
Diabetes can cause cardiovascular disease
There are several ways poorly controlled diabetes causes cardiovascular disease.
One of the ways diabetes contributes to cardiovascular disease is through high blood sugar levels. Elevated glucose levels in the blood can damage the blood vessels and increase the risk of cardiovascular disease. High blood sugar levels can cause oxidative stress, damaging the blood vessels and leading to cardiovascular diseases.
Another mechanism by which diabetes contributes to cardiovascular disease is inflammation. Chronic inflammation is a common feature of diabetes, increasing the risk of cardiovascular disease. Inflammation can cause damage to the blood vessels, making them more vulnerable to disease.
Diabetes can also lead to cardiovascular disease by causing abnormal lipid levels, including high LDL cholesterol and triglycerides. High levels of these lipids can increase the risk of heart disease and stroke.
High blood pressure is another common complication of diabetes, increasing the risk of heart disease and stroke. People with diabetes are more likely to have high blood pressure, which can damage the blood vessels and increase the risk of cardiovascular disease.
Diabetes damages Kidneys
Poorly controlled diabetes is a leading cause of kidney disease, and people with diabetes have a higher risk of developing kidney disease than those without diabetes.
One of the main ways diabetes causes kidney damage is by damaging the small blood vessels in the kidneys, called glomeruli. These blood vessels filter waste products from the blood, and when damaged, they can no longer properly filter the blood. This can lead to a build-up of waste products in the blood and a decline in kidney function.
Another way diabetes can cause kidney damage is by increasing the risk of developing high blood pressure. High blood pressure can damage the blood vessels in the kidneys (in glomeruli) and lead to a decline in kidney function.
In addition, diabetes can cause the kidneys to overwork, leading to inflammation and scarring in the kidneys. This can further damage the kidneys and decrease their ability to function correctly.
Nerve damage can occur with poorly controlled diabetes
People with poorly controlled diabetes have a higher risk of developing diabetic neuropathy than those without diabetes.
High blood sugar levels can damage the small blood vessels that supply blood to the nerves, leading to a decline in the amount of oxygen and nutrients that reach the nerves. This can cause the nerves to malfunction, leading to numbness, tingling, and pain.
Another way diabetes can cause nerve damage is by increasing the risk of developing high blood pressure. High blood pressure can damage the blood vessels that supply blood to the nerves, leading to a decline in the amount of oxygen and nutrients that reach the nerves.
In addition, diabetes can cause the nerves to become inflamed, further damaging the nerves and leading to a decline in their function.
Diabetic neuropathy can affect different nerves in different ways, depending on the type of neuropathy. There are several types of diabetic neuropathy, such as peripheral neuropathy, autonomic neuropathy, proximal neuropathy and focal neuropathy.
Poorly controlled diabetes causes damage to eyes
Diabetes-related eye problems, also known as diabetic retinopathy, are a common complication of diabetes.
It is estimated that up to 45% of people with diabetes have some degree of diabetic retinopathy. The risk of developing diabetic retinopathy increases with the duration of diabetes and with poor blood sugar control.
High blood sugar levels can damage the small blood vessels in the retina, which is the light-sensitive part of the eye. The damage causes leakage of blood and fluid, swelling and deposits of fatty material, which can affect vision.
Another way diabetes can cause eye damage is by increasing the risk of developing high blood pressure. High blood pressure can damage the blood vessels in the retina, leading to a decline in the amount of oxygen and nutrients that reach the retina.
In addition, diabetes can cause the retina to become inflamed, further damaging the retina and leading to a decline in its function.
Diabetic retinopathy has several stages, from mild to severe. It can be categorised into two main types: non-proliferative diabetic retinopathy, NPDR, and proliferative diabetic retinopathy, PDR.
NPDR is an early stage of the disease. It is characterised by small areas of balloon-like swelling in the retina, called microaneurysms, and tiny blood vessel leakage, called dot and blot haemorrhages. PDR is a more advanced stage, characterised by the growth of new blood vessels in the retina and can lead to severe vision loss.
High blood sugar causes foot damage
Diabetes can cause many problems for the feet if it is poorly controlled and lacks proper foot care.
High blood sugar levels can damage the blood vessels in the feet. In addition, high cholesterol levels cause problems such as poor circulation, a condition known as peripheral arterial disease. This can make it difficult for the feet to heal after an injury and increase the risk of infections.
Diabetes can also cause nerve damage, which affects the nerves that supply the feet. This can cause numbness, tingling, and pain in the feet. Numbness in the feet can make it difficult for a person to feel injuries or blisters, leading to infections and slow healing.
In addition, diabetes can cause the feet to become dry and cracked, leading to skin infections. Diabetes can also cause the skin on the feet to become thick and hard, leading to calluses and corns.
Another complication is Charcot foot. It’s a condition when the bones in the foot become weak and brittle and can fracture or displace easily. It’s caused by nerve damage and poor circulation, common in people with diabetes. Charcot foot can lead to severe deformities, making walking or wearing shoes difficult.
It weakens your immune system
Diabetes does not directly weaken the immune system, but poorly controlled diabetes can lead to a higher risk of infections and complications.
High blood sugar levels can damage the small blood vessels that supply blood to the immune system, leading to a decline in the amount of oxygen and nutrients that reach the immune system. This can make fighting infections and illnesses more difficult for the immune system.
Diabetes can also cause inflammation, further weakening the immune system. This chronic inflammation can lead to a state of immune dysfunction. As a result, it can make the person more susceptible to infections and illnesses.
In addition, diabetes can affect the function of specific white blood cells, which are an essential part of the immune system. These cells help the body to fight off infections and illnesses. When they are not functioning correctly, it can make the person more susceptible to infections and illnesses.
Diabetes can cause sexual problems in males and females
High blood sugar levels cause sexual problems in both males and females. In men, diabetes can cause erectile dysfunction (ED). This can be due to nerve damage, poor blood flow, or both.
In women, diabetes can cause sexual dysfunction, including difficulty becoming aroused, vaginal dryness, and pain during intercourse.
Diabetes can also affect the sexual health of women by leading to problems with the vaginal area, such as yeast infections, which can cause itching and burning.
Furthermore, nerve damage caused by diabetes can make it difficult to feel sexual pleasure.
What measures need to be taken to minimise diabetes complications?
Positive lifestyle measures, regular monitoring and adherence to prescribed medications can minimise complications.
- Tight control of blood sugar levels: Monitoring blood sugar levels regularly and taking steps to keep them within a healthy range can help prevent or slow the progression of complications.
- Regular physical activity: Regular exercise can help control blood sugar levels and reduce the risk of complications.
- Healthy eating: Eating a healthy diet low in saturated and trans fats, cholesterol, salt, and added sugars can help control blood sugar levels and reduce the risk of complications.
- Regular check-ups: Regular check-ups with a healthcare provider can help detect and manage diabetes complications early. This includes routine eye exams, foot exams, and screenings for cardiovascular disease.
- Medications: Taking medications as prescribed by a healthcare provider can help control blood sugar levels and reduce the risk of complications.
- Smoking and drinking alcohol: Quit smoking and limit alcohol intake, as smoking and drinking can cause or worsen diabetes complications.
- Maintaining a healthy weight: Losing and maintaining a healthy weight can help control blood sugar levels and reduce the risk of complications.
- Regular screening for diabetes-related complications, such as kidney, nerve and cardiovascular damage.
The Bottom Line
Diabetes is a serious condition that can lead to several complications if blood sugar is not vigorously controlled.
By understanding the potential complications, regularly monitoring blood sugar levels, following a healthy lifestyle and working closely with a healthcare provider, individuals with diabetes can reduce their risk of complications and improve their overall health.