Key Insight High cholesterol, or dyslipidaemia, means the fats in your blood are not balanced. The main types are LDL (bad cholesterol), HDL (good cholesterol), and triglycerides. High LDL and triglycerides can lead to heart disease and stroke by causing plaque in your arteries. Most people do not notice symptoms until serious issues develop, so regular blood tests matter. Causes include genetics, eating too many foods with saturated fats, lack of exercise, smoking, and drinking too much alcohol. Treatment often involves eating more vegetables, whole grains, and healthy fats, cutting back on red meat and processed foods, exercising, and sometimes taking medicines like statins. Small, steady changes can improve your cholesterol in a few weeks. |
Most people do not think about cholesterol until a blood test shows it is high. You can feel healthy and still have high cholesterol, which slowly increases your risk of heart disease and stroke.
Doctors call abnormal cholesterol levels dyslipidaemia. It is very common and affects millions of people worldwide. The issue is that it usually does not cause clear symptoms at first. By the time you notice problems, your arteries may already be affected.
Understanding cholesterol and why balance matters can help you protect your health over time. The good news is you can often improve your cholesterol by changing your daily habits, with or without medicine.
What Is Cholesterol and Why Does Balance Matter?
Cholesterol is a waxy, fat-like substance your body needs to build cells and make certain hormones. Your liver produces most of the cholesterol in your body, and you get some from food.
The issue is not cholesterol itself, but the balance of its different types in your blood. Cholesterol travels in your body attached to proteins called lipoproteins. These act like delivery trucks, carrying cholesterol where it is needed.
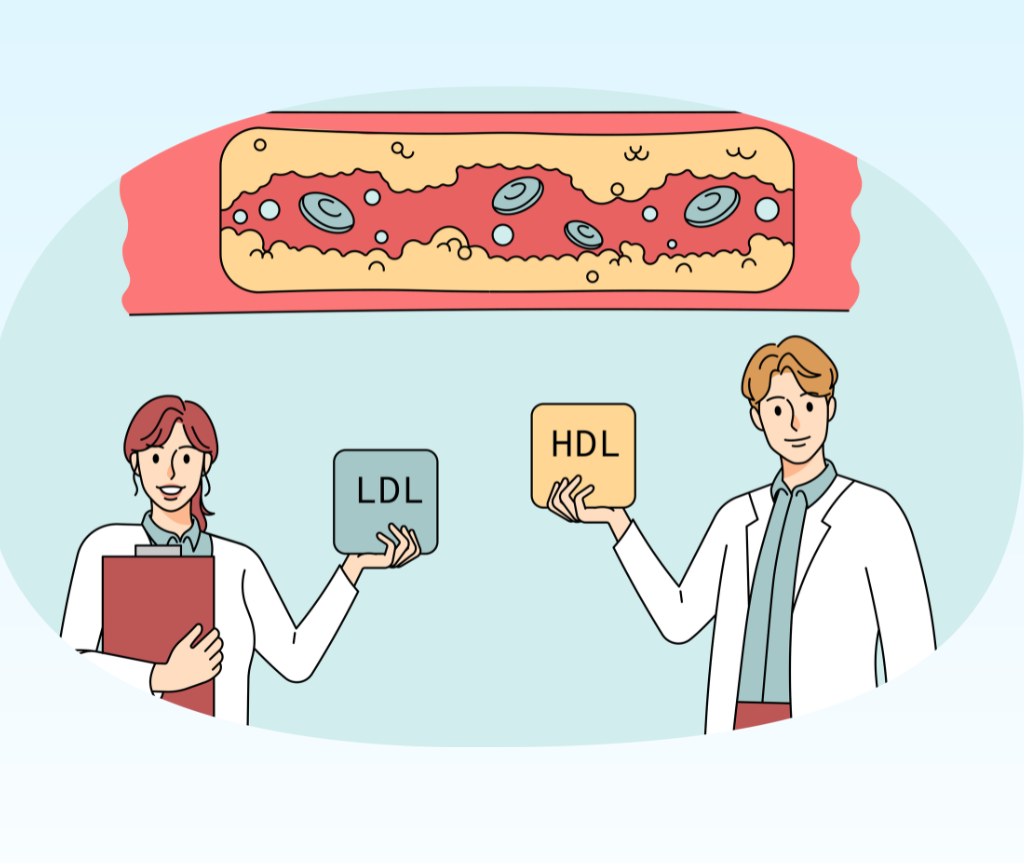
There are three main types to know about. LDL, or low-density lipoprotein, is called “bad” cholesterol because it can build up in your arteries and form plaque. HDL, or high-density lipoprotein, is “good” cholesterol because it helps remove extra cholesterol from your blood. Triglycerides are another kind of fat in your blood that can raise your risk of heart disease if the levels are too high.
If your LDL and triglycerides are too high, or your HDL is too low, you have dyslipidaemia. This imbalance increases your risk of hardened arteries, heart attack, and stroke.
Different Patterns of High Cholesterol
Dyslipidaemia is not just one problem. It can show up in different ways, depending on which blood fats are out of balance.
Hypercholesterolaemia means your total cholesterol is high, usually because your LDL is high. Hypertriglyceridaemia means your triglycerides are high. Mixed hyperlipidaemia means you have both high LDL and high triglycerides at once.
Each pattern gives doctors clues about what is happening in your body and helps them choose the best treatment.
What Causes High Cholesterol?
Many things affect your cholesterol levels. Some you can change, and others are inherited.
1. Genetics
Your genes play a significant role in how your body handles cholesterol. Some people inherit variations that affect the receptors on liver cells that pull LDL cholesterol out of the blood. When these receptors don’t work properly, LDL builds up even when you eat well and exercise regularly.
Familial hypercholesterolaemia (FH) is the most common genetic cause of very high cholesterol. People with FH can have LDL levels two to three times higher than normal, sometimes from childhood. If one parent has FH, you have a 50% chance of inheriting it.
The challenge is that FH often goes undiagnosed.
Many people do not know they have it until they get heart disease earlier than expected. If your family has a history of early heart attacks (before age 55 in men, 65 in women) or very high cholesterol, tell your doctor. You may need screening before age 40.
2. Diet
What you eat directly affects your cholesterol. The biggest dietary culprits are saturated fats, which raise LDL cholesterol by affecting how your liver processes fats.
Foods high in saturated fat include red meat, full-fat dairy products, processed meats like bacon and sausages, and baked goods made with butter or shortening. Your liver responds to saturated fat by producing more LDL particles and reducing the number of LDL receptors, which means more cholesterol stays in your blood.
Trans fats are even worse. They not only raise LDL but also lower HDL. Check ingredient labels for “partially hydrogenated oils,” which is another name for trans fats.
However, not all fats are harmful. Unsaturated fats from olive oil, avocados, nuts, and oily fish can actually improve your cholesterol balance. Soluble fiber from oats, beans, lentils, and apples also helps by removing cholesterol before it enters your bloodstream.
It is important to know that diet changes help, but they have limits. If you have genetic factors or certain health conditions, eating well might only lower your LDL by 10-15%. Some people need medicine even with a good diet, and that is normal.
3. Physical Inactivity
Being inactive affects your cholesterol in several ways that build on each other. It lowers your HDL cholesterol, makes it harder to maintain a healthy weight, and changes how your body processes fats. Studies show that sedentary people typically have HDL levels 10-15% lower than active people.
Exercise affects enzymes that control fat metabolism. When you’re active regularly, your body produces more of an enzyme called lipoprotein lipase, which breaks down triglycerides. Without regular activity, triglycerides build up in your blood.
The type of exercise is less important than being consistent. Research shows that 150 minutes per week of moderate activity (about 30 minutes, five days a week) can raise HDL by 5-10% and lower triglycerides by 10-20%. Improvements happen gradually. You might see changes in triglycerides in a few weeks, but HDL increases usually take two to three months.
4. Smoking
Smoking affects your cholesterol in two main ways. First, it damages the lining of your blood vessels, increasing the likelihood that they will accumulate fatty deposits. Second, it lowers your HDL cholesterol by about 10-15%.
Having both high cholesterol and smoking is especially risky. If you have both, your chance of heart disease is much higher than with just one factor. When you quit smoking, your HDL levels start to improve within weeks, and after a year, your risk of heart disease drops by about half.
5. Excess Weight
Carrying extra weight, especially around your middle, can affect cholesterol levels through several mechanisms. Visceral fat (the fat stored around your organs) releases substances that interfere with how your body processes fats. This increases LDL and triglyceride production while lowering HDL.
The good news is that losing 5-10% of your body weight can lower LDL by 5-8% and raise HDL by about 5%. For someone who weighs 90kg, losing just 4.5-9kg can make a real difference. These improvements usually take a few months of steady weight loss.
6. Alcohol
The relationship between alcohol and cholesterol is complicated. Small amounts might raise HDL slightly in some people, but even moderate drinking can significantly increase triglycerides.
When you drink alcohol, your liver focuses on processing it instead of managing fats. This can cause triglycerides to build up in your blood. Drinking heavily (more than 14 units per week) often raises both triglycerides and LDL cholesterol.
If your cholesterol test shows high triglycerides, your doctor will likely ask about your alcohol intake. In many cases, cutting back on drinking or stopping altogether can bring triglyceride levels down significantly within a few weeks.
7. Other Health Conditions
Several health conditions disrupt how your body makes or processes cholesterol. Type 2 diabetes affects cholesterol through insulin resistance, often creating a pattern of high triglycerides, high LDL, and low HDL. Improving blood sugar control usually improves cholesterol levels, too.
Underactive thyroid (hypothyroidism) slows the breakdown of LDL cholesterol, leading to its buildup in your blood. Treating hypothyroidism with thyroid hormone replacement often brings cholesterol back to normal.
Chronic kidney disease and polycystic ovary syndrome (PCOS) also affect cholesterol balance. If you have any of these conditions, treating them is often the first step toward better cholesterol levels.
Why High Cholesterol Causes No Symptoms
One of the hardest parts about high cholesterol is that it usually has no symptoms. Most people feel normal.
You might feel a bit tired sometimes, but these signs are easy to miss.
The real danger begins when high LDL and triglycerides cause plaque to build up in your arteries. This process, called atherosclerosis, happens slowly over many years. You will not notice it until blood flow is seriously reduced.
Symptoms only appear when atherosclerosis causes other problems. Chest pain or pressure during exercise can mean blocked heart arteries. Leg pain while walking may be a sign of arterial disease in your legs. Sudden weakness or confusion could be a sign of a stroke.
This is why regular cholesterol checks are important, even if you feel healthy. Testing can find problems early, when changing your habits or taking medicine can still prevent serious issues.
How High Cholesterol Is Diagnosed
Doctors check for high cholesterol with a fasting lipid profile. This blood test measures your LDL, HDL, triglycerides, and total cholesterol. You usually need to fast for 9 to 12 hours before the test to get accurate triglyceride results.
The NHS recommends that healthy adults have their cholesterol checked every 5 years from age 40. You may need more frequent testing if you have risk factors like family history of heart disease, diabetes, high blood pressure, smoking, or obesity.
Your doctor will look at your cholesterol results, along with other risk factors, to assess your overall heart risk. Having high cholesterol plus diabetes or high blood pressure is much riskier than high cholesterol alone.
Treatment Options That Work
Treating high cholesterol usually involves making lifestyle changes and taking medicine if needed. Even small, steady improvements can lower your risk of heart disease.
1. Dietary Changes
Changing your diet is often the first step. A heart-healthy diet includes lots of vegetables, fruits, whole grains, beans, and fiber-rich foods. These foods help lower LDL cholesterol naturally.
Choose healthier fats from sources like olive oil, avocados, nuts, seeds, and fatty fish. These unsaturated fats help balance your cholesterol levels. Omega-3 fatty acids from salmon, mackerel, sardines, flaxseeds, and walnuts are particularly beneficial.
Cut down on saturated fats by choosing lean meats, removing the skin from poultry, and using low-fat or fat-free dairy. Try to eat fewer processed, baked, and fried foods.
You do not have to be perfect. Small changes help. Try olive oil instead of butter. Eat fish twice a week instead of red meat. Snack on a handful of nuts instead of biscuits.
3. Regular Exercise
Exercise raises your HDL cholesterol and helps lower LDL and triglycerides. Try to get at least 150 minutes of moderate aerobic activity each week. This can be brisk walking, cycling, swimming, or any activity that gets your heart rate up.
You do not need a gym membership or special equipment. A 30-minute walk each day works for most people. As you get fitter, you can walk faster or longer, but being consistent matters more than how hard you exercise.
If your body weight is high, changing your diet and exercising together can help you lose weight, which also improves your cholesterol.
3. Medication
If lifestyle changes do not lower your cholesterol enough, medication can help. Your doctor will consider your overall heart risk, not just your cholesterol numbers, to decide whether you need medicine.
Statins are the most common medicine for high cholesterol. They block an enzyme your liver uses to make cholesterol, thereby lowering LDL levels significantly. Most side effects are mild, but some people get muscle pain.
If you have any concerns, talk to your doctor.
Other medicines include fibrates, which lower triglycerides, bile acid sequestrants, which block cholesterol absorption, and PCSK9 inhibitors for people who cannot take statins. Omega-3 supplements can also help if your triglycerides are very high.
Many people take long-term medicine to keep cholesterol under control. This does not mean lifestyle changes are not important. Combining medicine with healthy habits gives you the best results.
Managing High Cholesterol Long-Term
High cholesterol is not a life sentence. It means you can make changes to protect your health. Whether your cholesterol is a little high or much higher, you have ways to lower your risk.
The steps you take to improve your cholesterol also help your overall health. Eating better, moving more, keeping a healthy weight, not smoking, and drinking less alcohol lowers your risk of diabetes, some cancers, and other health problems.
Small, steady habits matter more than big changes you cannot keep up. Start with one adjustment. You might add a daily walk or swap butter for olive oil. After a few weeks, add another change. Let improvements build over time.
Most people see improvements in cholesterol within 6-12 weeks of making lifestyle changes. Your doctor will retest your levels to track progress and adjust treatment if needed.
Your cholesterol levels do not now determine your future. With the right information, support, and steady effort, you can improve your balance and protect your heart for years to come.